Yes, vagus nerve trauma can manifest with delayed symptoms after a car accident. While some injuries present immediately, others, particularly those involving the vagus nerve, can have a delayed onset of vagal nerve injury symptoms due to factors like inflammation, ongoing irritation, or the body’s initial response masking the full extent of the damage.
Car accidents are a common cause of physical trauma, and while the immediate impact is often obvious with broken bones or lacerations, less visible injuries can develop over time. One such area of concern is the vagus nerve, a critical component of the autonomic nervous system. This extensive nerve plays a vital role in regulating a wide range of bodily functions, from heart rate and digestion to mood and immune response. Damage to this nerve, often referred to as vagal nerve damage or vagal neuropathy, can lead to a variety of debilitating issues that may not appear until days, weeks, or even months after the initial event. This article delves into how post-accident nerve damage, specifically affecting the vagus nerve, can be delayed and what signs to look out for.
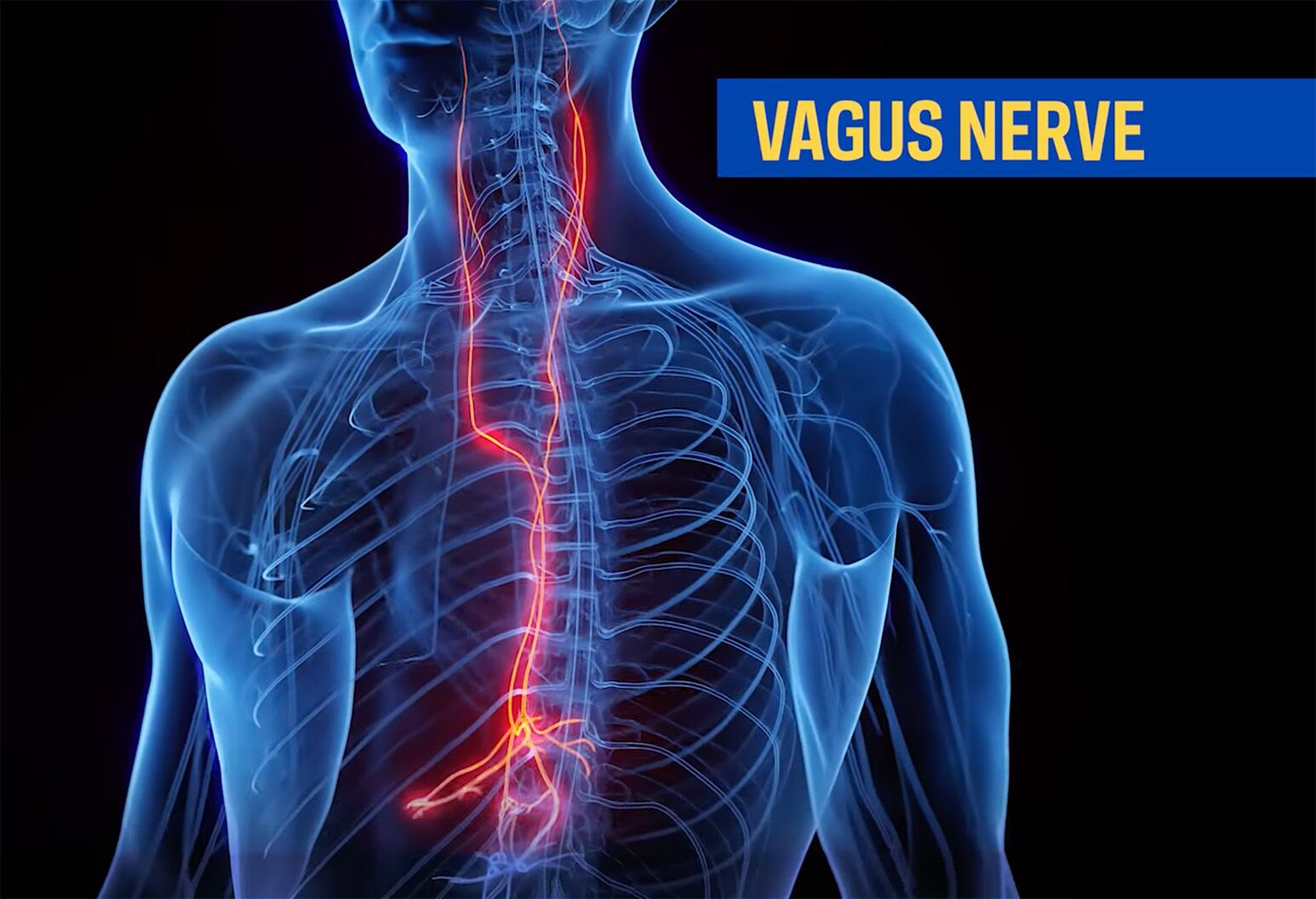
Image Source: dam.northwell.edu
Deciphering Vagus Nerve Trauma Following an Accident
The vagus nerve, the tenth cranial nerve, is the longest and most complex of the cranial nerves. It extends from the brainstem down through the neck, chest, and abdomen, connecting to numerous organs. Its broad reach means that trauma affecting any part of this pathway can lead to delayed vagus nerve dysfunction.
Mechanisms of Injury
During a car accident, the sudden acceleration and deceleration forces can subject the body to immense stress. These forces can cause:
- Direct Compression: The vagus nerve can be compressed by swelling, hematomas (blood clots), or displaced tissues around the neck or chest.
- Stretching and Tearing: The rapid movements can stretch or even tear nerve fibers, disrupting their ability to transmit signals.
- Inflammation: The body’s natural inflammatory response to injury can put pressure on the nerve, leading to delayed symptom onset.
- Vascular Compromise: Damage to blood vessels supplying the vagus nerve can impair its function.
Why Symptoms Might Be Delayed
Several factors contribute to the delayed presentation of vagus nerve issues after an accident:
- Body’s Initial Shock Response: Immediately after an accident, the body releases adrenaline and other stress hormones, which can temporarily mask pain and other subtle symptoms.
- Gradual Swelling and Inflammation: Edema (swelling) can take time to develop and can gradually compress the vagus nerve, leading to a slow progression of symptoms.
- Nerve Regeneration and Scar Tissue: If nerve fibers are damaged, the healing process can be slow. Scar tissue formation can also interfere with nerve signal transmission over time.
- Intermittent Symptoms: Vagus nerve symptoms can sometimes be intermittent, meaning they come and go. This can make it difficult to attribute them to the accident initially.
- Misattribution of Symptoms: Many vagus nerve symptoms, such as digestive upset or fatigue, are common and can be easily attributed to stress or other minor ailments, delaying a proper diagnosis.
Recognizing Vagal Nerve Injury Symptoms
The range of vagal nerve injury symptoms can be diverse, reflecting the nerve’s widespread influence. These symptoms can affect multiple bodily systems and may include:
Gastrointestinal Issues
The vagus nerve is heavily involved in regulating digestion. Damage can lead to:
- Gastroparesis: Delayed stomach emptying, causing nausea, vomiting, feeling full quickly, abdominal pain, and bloating.
- Dysphagia: Difficulty swallowing, which can manifest as choking or coughing during meals.
- Altered Bowel Habits: Changes in digestion can lead to constipation, diarrhea, or irregular bowel movements.
Cardiovascular Effects
The vagus nerve helps regulate heart rate. Symptoms can include:
- Bradycardia: A slow heart rate.
- Orthostatic Intolerance: Dizziness or fainting upon standing due to a drop in blood pressure.
- Arrhythmias: Irregular heartbeats.
Respiratory and Laryngeal Symptoms
The vagus nerve controls muscles in the voice box and airways. This can result in:
- Hoarseness or Voice Changes: Due to vocal cord paralysis or weakness.
- Breathing Difficulties: In severe cases, affecting airway control.
Other Potential Symptoms
- Dizziness and Vertigo: Disruptions in the autonomic nervous system can impact balance.
- Fatigue: Persistent and unexplained tiredness.
- Anxiety and Depression: The gut-brain axis, heavily influenced by the vagus nerve, can be disrupted, affecting mood.
- Somatic Symptoms: The body can manifest distress through physical symptoms without a clear organic cause, sometimes referred to as somatic symptom disorder after accident.
Post-Accident Nerve Damage Beyond the Vagus Nerve
While focusing on the vagus nerve, it’s crucial to acknowledge that car accidents can cause a broader spectrum of post-accident nerve damage. The somatic nervous system trauma can affect nerves controlling voluntary movement and sensation, leading to:
- Numbness and Tingling: Often in the extremities, indicating damage to peripheral nerves.
- Muscle Weakness or Paralysis: Affecting limbs or specific muscle groups.
- Pain: Including sharp, shooting pain or a persistent dull ache. In some cases, this can manifest as phantom limb pain after accident, even without actual limb loss, due to nerve misfiring.
- Loss of Sensation: Difficulty feeling touch, temperature, or pressure.
The autonomic nervous system dysfunction car accident victims experience is complex, impacting both the sympathetic (fight-or-flight) and parasympathetic (rest-and-digest) branches. The vagus nerve is the primary component of the parasympathetic system. Dysfunction in this system can manifest in many ways, contributing to the broad range of symptoms seen after trauma.
The Interplay with Psychological Trauma
It’s essential to consider the psychological impact of a car accident. Post-traumatic stress disorder nerve symptoms can overlap with physical nerve damage. The heightened state of arousal, anxiety, and altered sensory processing associated with PTSD can mimic or exacerbate nerve-related complaints. Trauma can deeply affect the nervous system, leading to both physical and psychological manifestations. Chronic stress can also contribute to inflammation and pain, potentially worsening any existing nerve issues.
When to Seek Medical Attention
Given the potential for delayed symptoms, it’s vital for anyone involved in a car accident to undergo a thorough medical evaluation, even if they feel fine initially. Any new or persistent symptoms that arise after an accident should be reported to a healthcare professional.
Key indicators that warrant immediate medical attention include:
- Sudden onset of severe dizziness or fainting.
- Difficulty swallowing or breathing.
- Chest pain or palpitations.
- Unexplained nausea or vomiting that persists.
- Significant changes in bowel or bladder function (e.g., neurogenic bladder after accident, where nerve damage affects bladder control).
Diagnosing Delayed Vagus Nerve Trauma
Diagnosing delayed vagus nerve dysfunction can be challenging due to the often vague and overlapping nature of the symptoms. A comprehensive approach is necessary, typically involving:
Medical History and Physical Examination
A detailed history of the accident and a thorough physical examination are the first steps. The doctor will ask about:
- The nature of the accident and any reported injuries.
- The onset and progression of symptoms.
- Any pre-existing medical conditions.
The physical exam will focus on neurological signs, cardiovascular function, and gastrointestinal assessment.
Diagnostic Tests
Several tests can help confirm vagus nerve damage and rule out other conditions:
- Esophageal Manometry: Measures the muscle contractions in the esophagus and the tone of the lower esophageal sphincter, providing insights into vagal nerve control over swallowing and digestion.
- Gastric Emptying Scans: Assesses how quickly food leaves the stomach.
- Electrocardiogram (ECG) and Holter Monitoring: To evaluate heart rate and rhythm.
- Tilt Table Test: To assess the body’s response to changes in posture, helpful in diagnosing autonomic nervous system dysfunction car accident patients.
- Electromyography (EMG) and Nerve Conduction Studies: While typically used for peripheral nerves, specialized tests might be used to assess certain aspects of vagal nerve function, though direct testing of the vagus nerve is complex.
- Imaging Studies: MRI or CT scans of the neck and chest might be used to rule out structural causes of nerve compression, such as a herniated disc or hematoma.
Management and Treatment Strategies
The treatment for vagus nerve trauma depends on the severity and specific symptoms. The goal is to alleviate symptoms, improve nerve function, and manage any underlying complications.
Medical Treatments
- Medications:
- Prokinetics: Drugs that help speed up gastric emptying (e.g., metoclopramide, domperidone).
- Anti-nausea medications: To manage vomiting.
- Medications for cardiovascular symptoms: Such as beta-blockers or fludrocortisone for orthostatic intolerance.
- Dietary Modifications:
- Small, frequent meals: To ease the burden on a slow stomach.
- Low-fat, low-fiber diet: Can help improve digestion.
- Hydration: Crucial for overall bodily function.
Lifestyle Adjustments
- Regular, gentle exercise: Can improve circulation and overall well-being.
- Stress management techniques: Yoga, meditation, and mindfulness can help regulate the autonomic nervous system.
- Avoiding triggers: Identifying and avoiding foods or situations that worsen symptoms.
Therapies
- Vagal Nerve Stimulation (VNS): In some cases, electrical stimulation of the vagus nerve, typically implanted surgically, can be used to treat conditions like epilepsy and depression, and research is ongoing for other vagal nerve-related issues. Non-invasive vagus nerve stimulators are also becoming available.
- Speech Therapy: For individuals experiencing dysphagia or hoarseness.
- Physical Therapy: To help manage pain, improve mobility, and address any associated musculoskeletal issues.
Psychological Support
Given the potential overlap with psychological trauma and the impact on quality of life, psychological support is often crucial. Therapy can help individuals cope with the chronic pain, anxiety, and depression that can accompany chronic pain after car crash and nerve damage. Cognitive Behavioral Therapy (CBT) and Eye Movement Desensitization and Reprocessing (EMDR) are often effective.
Table: Potential Delayed Symptoms and Related Issues
| Symptom Category | Potential Delayed Vagus Nerve Symptoms | Associated Conditions |
|---|---|---|
| Gastrointestinal | Nausea, vomiting, early satiety, bloating, abdominal pain, constipation | Gastroparesis, dysphagia, irritable bowel syndrome-like symptoms |
| Cardiovascular | Dizziness upon standing, fainting, palpitations, slow heart rate | Orthostatic intolerance, vasovagal syncope |
| Respiratory/Voice | Hoarseness, chronic cough, difficulty swallowing | Vocal cord paresis/paralysis, aspiration risk |
| Neurological | Persistent fatigue, anxiety, mood changes, general malaise | Somatic symptom disorder, impact on mental health due to gut-brain axis disruption |
| Urinary | Difficulty initiating urination, incomplete bladder emptying | Neurogenic bladder after accident (if sacral nerves are also affected or autonomic) |
| Pain | Persistent localized or diffuse pain | Chronic pain after car crash, potentially amplified by nerve dysfunction and inflammation |
Case Study Illustration (Hypothetical)
Consider a patient, Sarah, who was in a moderate-speed car accident. She initially felt sore but otherwise functional. A week later, she started experiencing significant nausea and felt full after eating only a few bites. Over the next month, she developed severe abdominal bloating, constipation, and occasional dizziness when standing up. Her primary care physician initially attributed these to stress. However, the persistence and severity of her symptoms prompted a referral to a gastroenterologist, who, after further investigation including a gastric emptying study, diagnosed gastroparesis likely caused by vagus nerve damage sustained during the accident. This case highlights how delayed vagus nerve dysfunction can easily be missed if symptoms aren’t directly linked to the traumatic event.
Addressing Chronic Pain After a Car Crash
Chronic pain after car crash is a significant concern for many survivors. This pain can stem from multiple sources, including nerve damage, soft tissue injuries, and psychological factors. When the vagus nerve is affected, the resulting digestive issues, fatigue, and altered mood can contribute to or exacerbate the overall pain experience. The interconnectedness of the nervous system means that damage to one area can have ripple effects, impacting pain perception and the body’s ability to cope.
Navigating a Neurogenic Bladder After Accident
While the vagus nerve is primarily associated with the parasympathetic system controlling visceral organs, severe trauma can impact other parts of the nervous system, including the sacral nerves that control bladder function. This can lead to a neurogenic bladder after accident, characterized by difficulties with bladder control, retention, or incontinence. The presence of such symptoms, alongside potential vagus nerve issues, underscores the widespread impact of significant trauma on the entire nervous system.
Frequently Asked Questions (FAQ)
Q1: How long can it take for vagus nerve symptoms to appear after a car accident?
A1: Symptoms can appear anywhere from a few days to several weeks or even months after a car accident. This delay is often due to gradual swelling, inflammation, or the body’s initial compensatory mechanisms masking the injury.
Q2: What are the most common delayed symptoms of vagus nerve damage?
A2: The most common delayed symptoms involve the digestive system, such as nausea, feeling full quickly, bloating, and abdominal pain. Cardiovascular symptoms like dizziness upon standing and general fatigue can also appear later.
Q3: Can anxiety from a car accident cause vagus nerve symptoms?
A3: While anxiety itself can cause some vagal nerve-like symptoms (e.g., butterflies in the stomach), significant psychological trauma from an accident can also impact the autonomic nervous system, potentially exacerbating or contributing to delayed nerve dysfunction. It’s important to distinguish between stress-induced symptoms and actual nerve damage.
Q4: Is vagus nerve damage permanent after a car accident?
A4: The permanence of vagus nerve damage depends on the severity of the injury. Some nerve damage can heal over time, especially if it involves stretching rather than severing. However, severe or prolonged compression can lead to permanent functional impairment. Treatment and rehabilitation play a crucial role in recovery.
Q5: What should I do if I suspect I have delayed vagus nerve symptoms after an accident?
A5: If you experience persistent or new symptoms after a car accident, such as digestive problems, dizziness, or unexplained fatigue, it’s crucial to consult a healthcare professional. A thorough medical evaluation, including specialized tests, will help determine the cause and guide appropriate treatment.
Conclusion
The intricate pathways of the nervous system mean that trauma, like that sustained in a car accident, can have far-reaching and sometimes delayed consequences. Vagus nerve trauma is a prime example of how a critical nerve can be affected indirectly, leading to a cascade of symptoms that may not manifest immediately. Recognizing the potential for post-accident nerve damage and understanding the diverse range of vagal nerve injury symptoms, including those that appear later, is crucial for prompt diagnosis and effective management. If you have been involved in a car accident, be vigilant about any new or persistent bodily changes, and seek professional medical advice to ensure your health and well-being are fully addressed. Addressing the complexities of autonomic nervous system dysfunction car accident survivors face is key to a comprehensive recovery.